Defending as a whole person: is violation the only threat we care about?

Written by Johanna Lynch – University of Queensland
Our culture is cued into violence and action. Action heroes (and their medical counterparts in the emergency department) are highly visible and valued. Quieter things like patience and attention to detail or kindness to marginalised people are rarely featured in our entertainment. In the news, violence and fear are often on the front page while deep good things are ignored. In healthcare we see these attitudes in the funding models that gives millions to places of action (the hospital) and new ideas (like shiny new clinics) and the leftovers to parts of the health system that care for the poor and prioritise prevention. In general practice we see this in higher Medicare funding for procedures and fast consultations and lower funding for longer consultations and processes that take time to listen deeply, understand and care (like complex distress). This can also be seen in the reductive way that First Nations people are depicted in mainstream medica with a focus on violence and harm, and not on the deep gifts they have given our culture. I draw attention here to the First Nations values of ‘Dadirri’ : ‘inner deep listening and quiet still awareness’- in the Ngan’gikurunggurr and Ngen’giwumirri languages1p.14, and ‘Ngarraanga Giinganay ‘ – thinking peacefully in the language of Gumbaynggirr country.2
As well as action, our culture is wedded to measuring things. Our healthcare policy funding is cued into ‘evidence’ and ‘outcomes’ – which often is code for ‘easily measurable’. Being able to measure something easily has always been something that politicians need – tied into election cycles that need quick results that become easy sound bites. Turns out that this same attitude influences funding of research – in cycles needing evidence of public funding well spent. Louise Stone says this causes disease prestige – where care and research into easily measured diseases are more easily funded and prioritised.3 This means that diseases that can be seen (like cancer) or diseases that lead to procedures (eg. hip replacements or gastroscopies) or formulaic responses (like CBT), are prioritised (and made more commercially valuable) compared to complex psychosocial distress with quiet relational therapies that impact wellbeing across generations like community development, healing from trauma, or learning how to regulate emotion or parent well. Even more worrying – the word ‘evidence’ has schooled a generation of scientists and clinicians to search for measurements rather than a broader view of science, healing and health. A commonly used hierarchy of evidence has overvalued reductionist knowledge that can promise precise repeatable knowledge that predicts outcomes, and undervalued wisdom4 and healing that are often imprecise and difficult to measure, and yet deeply valuable.
This focus on action and measurement is not benign. Mixed with tight funding cycles, it skews clinical assessment processes and public funding models away from whole person wellbeing, early intervention, and prevention and towards easily identifiable disease and organ failure. It skews treatment away from whole of society prevention, invisible human kindness and comfort, and towards action in hospitalisation, procedures or pill-taking. It skews public attention away from invisible processes that harm (like emotional neglect) and towards overt actions that harm (like the many forms of assault). It also skews attention away from inner experiences and towards visible behaviours or physical impacts on a person. This is part of why the voice of people with lived experience in public policy is so important. Listening to and integrating the viewpoint of lived experience into public policy can help to reduce the focus on action and measurement and widen attention to the complexity of caring for a whole community.
The quieter more invisible processes that impact wellbeing can be written out of a story defined by narrow measurable events and actions. This includes an overvaluing of numbers compared with words – as though numbers are more real. Searching only for what can be measured impoverishes our understanding, makes our research unscientific, blinds us to subtle and complex strengths, and even reduces our capacity to innovate new ways to respond and care.
Those who study the impact of stressors on the physical body declare boldly that both unseen and seen harms have impacts we need to care about. Our human defenses are activated by both. Psychoneuroimmunologists Monika Fleshner and Mark Laudenslager assert:
“The disparity between physical and psychological stressors is only an illusion. Host defense mechanisms respond in adaptive and meaningful ways to both.”5p.114
So, those of us who are healers need to always remember that humans respond as an interconnected whole when defending against threat. Healers need to stay actively aware of the links between what is invisible and what is seen, what is loud and what is quiet, what is active and what is still, what is invasive and what is dismissive or disconnecting. We need to resist the draw towards only noticing action and what can be easily seen and measured.
I was reflecting on how the recent Olympics and Paralympics, could be seen as the ultimate place where action is measured! They also have a strong focus on outcomes in the form of world records and medals. Is that why we watch and cheer? Or is there something deeper and less visible going on when the world gathers to watch? Something that is perhaps even more visible at the Paralympics? Something about human dignity, passion, dedication, patience, respect, friendship, teamwork, spirit? The original values of Olympism were to “encourage effort”, “preserve human dignity” and “develop harmony”.6 Perhaps these are a beautiful immeasurable description of healthy community – perhaps that is why we cheer?
There are many drivers towards only searching for what is easily measurable. One of these is a misunderstanding about the nature of reality: a kind of materialistic philosophy where only what is observable is considered real. This narrows our conception of what it is to be human. It blinkers our attention and blinds us to other forms of reality that are not so visible. It lets us see shapes and colours while missing beauty and awe. It causes us to focus on observing the individual and so we miss their sense of self, hope, and connections to community and country. During the COVID-19 pandemic – it led to public policy that prioritised masks, without tuning in to the needs for children to learn to speak seeing human faces. It prioritised distance without addressing the deep importance of human longing for touch and connection. This focus on what can be measured elevates psychiatric conceptualisations of reality that focus on observable symptoms while having minimal conceptualisation of the role of lived experience, relationships, and even morality, including the hidden sicknesses of hatred, bitterness, envy, and fear. In the current social pandemics of hopelessness, loneliness, and interpersonal cruelty, it contributes to ‘trauma’ (the Greek word for ‘wound’) being narrowed through a psychiatric lens to only mean threatened physical life. This narrowed attention to action is part of why the complex invisible pain and harm inside families has been termed ‘domestic violence’, reducing attention to neglect, and the soul-crushing and invisible ways that humans can hurt each other without action or words.
Perhaps this is also why those who advocate for suicide prevention find it difficult to shift attention to invisible and complex contributors to suicide that require whole-of-government changes in attitude.7,8 It is perhaps why invisible drivers that thwart suicide prevention remain resistant to change, such as “commercial determinants” where unseen profit incentives damage community health,9 or stuck blocks to collaboration across university faculties or governmental departments that prevent unified innovation. For example, we have known that gambling is linked to suicide since 17907, but the way it tortures families and individuals, and the way its powerful lobby impacts public policy are largely invisible in psychiatric or health responses to suicidality.
In the words of one person with a lived experience of suicide: “To create a genuinely effective, sustainable approach to suicide prevention, we need to […] look at how we love, how we communicate, and how we treat others, especially those who are vulnerable, and our various systems – health, social, welfare, economic, education, and others – exacerbate or contribute to suicide.”10p.20 Even though it is invisible: how we love matters.
While I was designing my doctoral research methodology, I came across a division between objective understanding of reality (positivism)- the ‘what’s’ of life, and the subjective relational kind of knowledge that sees reality in culture, spirit, relationship and context (post-positivism) – the ‘who’s’, ‘how’s’, and ‘why’s’ of life.11,12 As a GP, I was searching for a way to see both kinds of knowledge that related to how I made clinical decisions in everyday practice. I discovered a kind of reciprocity or complementary match between positivist and post-positivist knowledge, which became the Whole Person Knowledge Map outlined below:
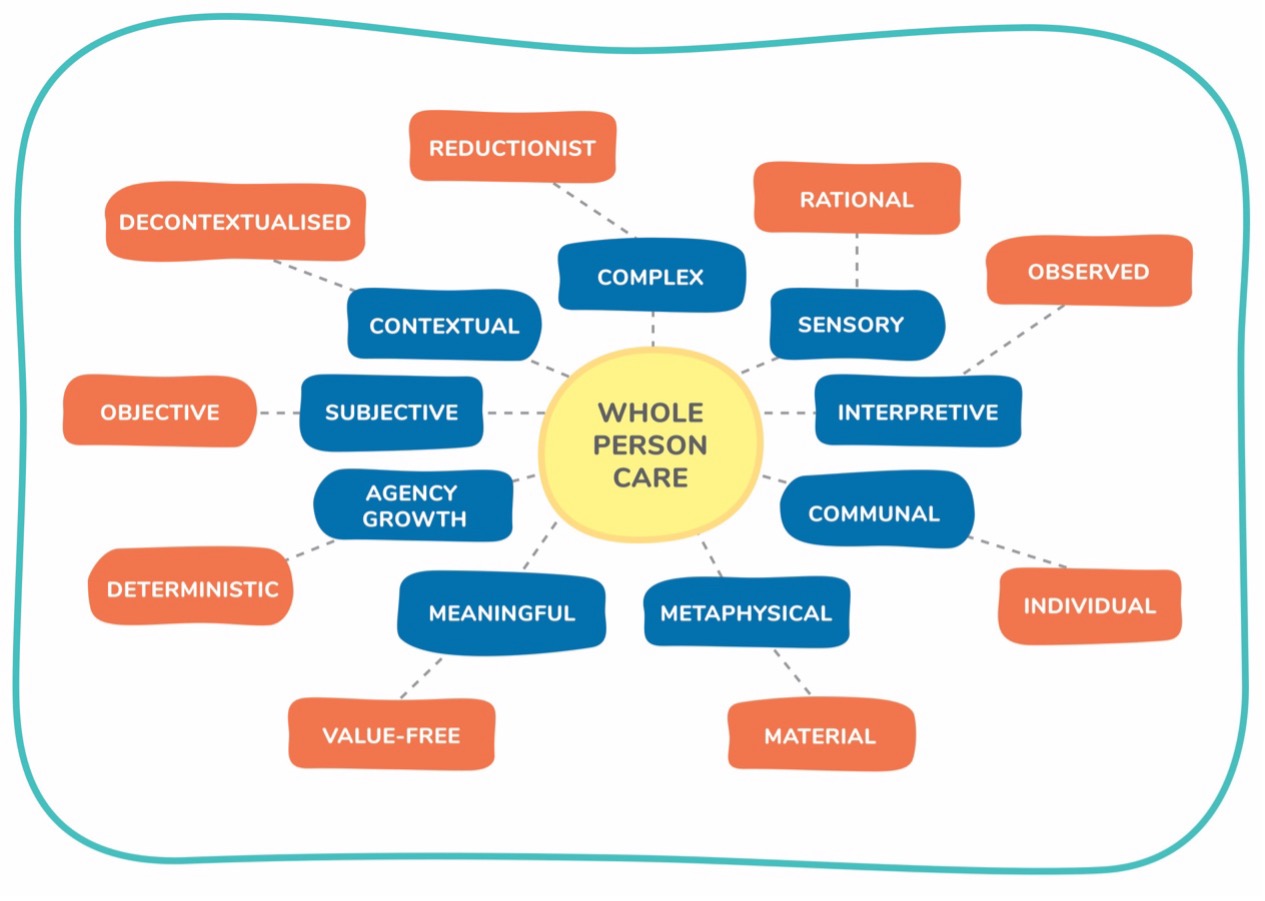
Figure 1: Whole Person Knowledge Map. Used with permission from Lynch, J.M. (2021) A Whole Person Approach to Wellbeing: Building Sense of Safety. Routledge: London (orange = positivist; blue = post-positivist)
This map helps us to see that both kinds of knowledge matter when we want to see a whole. Both are a kind of science – both see reality from different angles. Good quality care should bring them together so we can see the whole person. This map also helps us to see the limitations of positivist/reductionist knowledge – it is decontextualised, it is deterministic (this is why it is hard for the recovery movement to gain traction in psychiatry, and it is why a psychiatric diagnosis often sticks for a lifetime), and it is very individualised. It also shows the gifts of positivist knowledge – (links to objectivity, observation, and reason) and pos-positivist knowledge (awareness of context, sensation, relationships, movement, and meaning-making).
Measurement and action. These are visible and hard to ignore. Subjective relational and meaningful kinds of knowledge that are also part of health are more invisible and easier to ignore. It takes an act of resistance against dominant ways of seeing reality to notice all parts of the whole.
First Nations elders have been saying this for decades built on thousands of years of wisdom about the interconnectedness of place, people, spirit, and health.13,14 They invite us to listen deeply with a quiet still awareness (Dadirri). They remind us about country, community and spirit as part of health. In the words of elder Puggy Hunter:
“There is an urgent need to shift the paradigm of Aboriginal health service delivery away from the current maze of programs and specialists dealing with specific conditions, to a holistic approach that looks at the health of the whole person, family, and the community.
The ‘body parts’ approach has been a complete failure in Aboriginal health. There is no use treating the heart or the ears alone, when the whole person is in danger of breaking down… This means a new way of thinking.”15
General practitioners also call for a way of seeing people that cares for both their objective biology and their subjective biography.16 This generalist way of seeing highly values an expertise in whole person care that sees the unseen alongside the seen, the unpresentable alongside the presented concerns, the person inside their community.11,17-20 It even dares to question the ascendancy of the ‘evidence-based medicine’ that overvalues observation and undervalues the unseen, tacit, intuitive, spiritual and cultural ways of knowing.4,21,22 Generalism is a valued approach within family medicine, paediatrics, geriatrics, palliative care, social work, occupational therapy, and mental health nursing. Generalism is good at seeing all forms of suffering so that it can offer healing.
Valuing this kind of generalist and First Nations wisdom about the whole person could enrich clinical care and public policy.23
When we think about defending ourselves – of course people are cued into the invisible and the visible causes of threat. Of course, we have to defend the whole of ourselves. Of course, any strengths or suffering in our inner and outer worlds impacts the whole. Again, as Abraham Maslow reminds: threat impacts “a whole human being … never a part of a human being’.24p.75
In these essays we have reflected together on the whole ways that we sense, feel, experience, connect, and comfort one another. And here is another – the whole way that we defend ourselves. In each of these important human experiences, it is possible to ignore parts of a person that are essential for their healing. It is possible to fragment a whole just because it is easier to see the parts.
Noticing the wounds, threats, suffering, defences, sensations, strengths, and gifts of each person within their community and context is a way of resisting fragmentation. This is the active pattern recognition work of whole person care. Learning ways of being from First Nation’s wisdom about Dadirri (inner deep listening and quiet still awareness) and Ngarrangag Giinganay (thinking peacefully) could help us to see people and their strengths with our whole hearts.
The author would like to thank Dr Matthew Lewis for their review of an earlier draft.
- Ungunmerr MR, ed. Dadirri: Listening to One Another. Aboriginal and Torres Strait Islander Apostate, Catholic Archdiocese of Brisbane; 1993. Hendricks J, Heffernan G, eds. A Spirituality of Catholic Aborigines and the Struggle for Justice.
- Lavrencic LM, Donovan T, Moffatt L, et al. Ngarraanga Giinganay (‘thinking peacefully’): Co-design and pilot study of a culturally-grounded mindfulness-based stress reduction program with older First Nations Australians. Evaluation and Program Planning. 2021;87:101929.
- Stone L. Disease prestige and the hierarchy of suffering. Medical Journal of Australia. 2018;208(2):60-62.
- Reeve J. Scholarship-based medicine: teaching tomorrow’s generalists why it’s time to retire EBM. Br J Gen Pract. 2018;68(673):390-391.
- Fleshner M, Laudenslager ML. Psychoneuroimmunology: then and now. Behavioral and Cognitive Neuroscience Reviews. 2004;3(2):114-130.
- website IOC. Olympic values. Accessed 16 Sept 2024, 2024. https://olympics.com/ioc/olympic-values
- Pirkis J, Dandona R, Silverman M, Khan M, Hawton K. Preventing suicide: a public health approach to a global problem. The Lancet Public Health. 2024;
- Hawton K, Pirkis J. Preventing suicide: a call to action. The Lancet Public Health. 2024;
- van Schalkwyk MC, Collin J, Eddleston M, et al. Conceptualising the commercial determinants of suicide: broadening the lens on suicide and self-harm prevention. The Lancet Psychiatry. 2023;10(5):363-370.
- Shand F, Yip, D., Tye, M., Darwin, L. What can be done to decrease suicidal behaviour in Australia? A call to action. The impact on social determinants on suicide and how policy settings can help.chapter 2:17- 26. Accessed 16 Sept 2024. https://www.blackdoginstitute.org.au/wp-content/uploads/2020/09/What-Can-Be-Done-To-Decrease-Suicide_Chapter-2-Social-Determinants.pdf
- Lynch JM, van Driel, M., Dowrick, C.F., Meredith, P. Transdisciplinary Generalism: Conceptualising the clinical and research tasks of whole person care. presented at: North American Primary Care Conference; 2020;
- Lynch JM. Sense of Safety: a whole person approach to distress. University of Queensland; 2019.
- Gee G, Dudgeon P, Schultz C, Hart A, Kelly K. Aboriginal and Torres Strait Islander Social and Emotional Wellbeing. In: Dudgeon P, Milroy H, Walker R, eds. Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice. Commonwealth of Australia; 2014.
- Zubrick SR, Dudgeon P, Gee G, et al. Social determinants of Aboriginal and Torres Strait Islander social and emotional wellbeing. Working together. 2004;75
- Hunter PA. Searching for a new way of thinking in Aboriginal health. The Australian Health Consumer. 1999;2:16-17.
- Reeve J, Dowrick C, F., Freeman GK, et al. Examining the practice of generalist expertise: a qualitative study identifying constraints and solutions. JRSM Short Reports. 2013;4(12):1-9.
- Lynch JM, van Driel M, Meredith P, et al. The Craft of Generalism: clinical skills and attitudes for whole person care. Journal of evaluation in clinical practice. 2021;
- Reeve J. Wise GP: Championing the bananarama principle in general practice. Accessed 25/2/20, 2020. https://www.rcgp.org.uk/clinical-and-research/about/clinical-news/2019/october/wise-gp-championing-the-bananarama-principle-in-general-practice.aspx
- Lynch JM, Thomas HR, Askew DA, Sturman N. Holding the complex whole: Generalist philosophy, priorities and practice that facilitate whole-person care. Australian Journal of General Practice. 2023;52(7):428-433.
- Lynch JM. A Whole Person Approach to Wellbeing: Building Sense of Safety. Routledge; 2021
- Reeve J, Firth A. Revitalising general practice: unleashing our inner scholar. British Journal of General Practice. 2017;67(659):266-266.
- Reeve J. Protecting generalism: moving on from evidence-based medicine? Br J Gen Pract. 2010;60(576):521-523.
- Reeve J. Primary care redesign for person-centred care: delivering an international generalist revolution. Australian journal of primary health. 2018;24(4):330-336.
- Maslow AH. Motivation and Personality Third Edition. Harper Collins Publishers; 1954.
About the writer

Dr Johanna Lynch MBBS PhD FRACGP FASPM Grad Cert (Grief and Loss) is a retired GP who writes, researches, teaches, mentors and advocates for generalist and transdisciplinary approaches to distress that value complex whole person care and build sense of safety. She is an Immediate Past President and Advisor to the Australian Society for Psychological Medicine and is a Senior Lecturer with The University of Queensland’s General Practice Clinical Unit. She spent the last 15 years of her 25 year career as a GP caring for adults who are survivors of childhood trauma and neglect. She consults to a national pilot supporting primary care to respond to domestic violence.